Information Equals Life: The Future of Radiology IT
Inspiration often comes from unexpected places. Healthcare, as with military precision, relies on mission-critical decision making under uncertainty. Physicians, like top notch fighter pilots, are…

Inspiration often comes from unexpected places. Healthcare, as with military precision, relies on mission-critical decision making under uncertainty. Physicians, like top notch fighter pilots, are diligently trained for high-speed tasks in dynamic environments with imperfect information.
I believe an analytical model from aviation tactics can apply to healthcare. To teach aerial dogfighting tactics and increase survivability, strategist USAF Col. John Boyd introduced the OODA loop model in a 1977 briefing called Patterns of Conflict.
OODA is a nested set of loops for Observe, Orient, Decide, and Act, providing a framework for the entangled decision-making between a fighter pilot and an opponent pilot. Environmental observations are made. Orientation comes from integrating and synthesizing information from various sources. This leads to a decision and action. In an implicit nod to the Bayesians out there, these information sources include prior knowledge and experience.
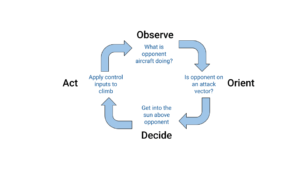
Boyd’s OODA loops have been applied to other domains due to the generality of modeling adversarial decision-making with uncertainty. In business, observations are made of both internal and external drivers of change in the market, strategic plans are oriented around these observations, and then decisions are made and acted upon to out maneuver the competition. In sports, they’re used to describe extremely fast decision-making processes at a play-by-play level, like calling an audible in football in response to defensive formations.
In healthcare, OODA loops have been used to model medical decision-making in response to therapy, but they haven’t yet surfaced in describing detailed workflows in diagnostic radiology. It’s past time to do so. But if we liken dictation of radiological findings to playing a game of hide and seek with lesions, then ‘search and describe’ is an apt moniker for observe/orient and decide/act.
We’ve seen radiology workflow models for disjointed IT components, like with the initiative for Integrating the Healthcare Enterprise (IHE):
- Patient registration and order entry in HIS.
- Order scheduling in RIS.
- Image acquisition by the modality.
- Image management and archival by PACS.
The catch is, this macro level workflow model is at the hours timescale but misses details at the micro level of a radiologist’s diagnosis, where the most dynamic flows are at the millisecond timescale.
In the Sirona radiology solution, we use a rational approach to identify and address inefficient constrictions in the flow. More cooperative than adversarial, intelligence amplification (IA) is used to get inside and beneficially shortcut the radiologist’s innermost loops. This underscores the power of deeply integrated components, such as Sirona’s unified approach to worklist, viewer, and reporter in one solution. You can see the nesting of loops – from 25 milliseconds to half a minute – in the radiology flow below, from worklist selection to report submission.
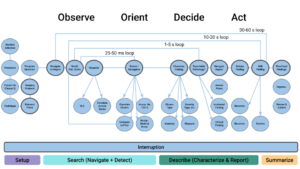
For example, our UX team maps out the user journey with highly detailed coding analyses of radiologist reading sessions. The designers document all of the individual steps in the interpretive cycle and validate the radiologist OODA model. This reveals crucial pain points (e.g., keeping eyes on image and efficient dictation) and a spectrum of user personas (e.g., Novelist, Rocket Scientist, Architect, and Minimalist). The fundamental bandwidth and cognitive processing limits of the human brain may be steadfast, but platform technology makes leaps and bounds with each new generation. The result? Radiologists freed from the diagnostic drag of sluggish tools and tedium.
Radiologists, like pilots, must make decisions quickly in dynamic environments. A sophisticated, cloud-based workflow is long overdue, and it’s time we give radiologists a modern cockpit worthy of their clinical prowess, delivering the right information at the right time and place. It’s been said of state of the art, fifth generation fighter aircraft such as the F-35 that “information equals life.” Doesn’t that sound just like radiology!